Are you tired of generic electronic medical record (EMR) software that doesn't quite fit your needs? Do you dream of a custom solution that can streamline your practice and save your sanity?
Look no further! In this article, we'll show you how to develop your very own custom EMR software, no coding experience required. Get ready to save your budget and your nerves with these tips from the experts.
EMR or EHR: What Type Is for You?
Gone are the times where physicians keep all the patients records manually. Since 2008 when the US President Barack Obama signed the act for the digitization of medical records, the number of vendors of electronic medical records solutions have been increasing exponentially.
In essence, both EMR (electronic medical records) and EHR (electronic healthcare records) mean the digital documentation of a medical facility that may consist of patient information, treatment plans, history and interactions with third-party services. Sometimes these terms are used interchangeably, but mostly professionals differentiate them.
Here some other distinctions:
- EMRs are supposed to be related mostly to inner use of a medical organization and their functionality is limited to patient profiles, diagnosis records and treatment tracking. EMRs usually do not support integration with third-party systems for data sharing outside the individual practice.
- EHR medical software includes more diverse features than EMRs. There are e-prescribing, advanced reporting, speech recognition, etc. The main difference from EMR is that EHR can support integrations with other software used within the organization or beyond to seamlessly exchange a patient’s data with laboratories, clinics and other specialists involved in the patient’s care. Data stored in EHR can travel with the patient wherever she goes - to another medical institution, state or country. An Electronic Medical Records software for a hospital mean that data stays in the specific medical institution and cannot be taken from it.
- Let’s go further and mention one more type - the personal health records (personal medical records software). This type relates to the medical records that are kept by the patient personally. Instead of doing it in paper, patient can use electronic version that is more than just a notepad. It can be equipped with many useful features, for instance X-ray, MRIs and other images storage and recognition. This can be personal or family health history that is in responsibility of a patient herself and, thus, can be kept in more informal format.
So, considering your requirements, you may have already defined which type of software mirrors best your organization’s needs.
Need EMR or EHR? Let’s estimate your project!
Contact UsBenefits of Using EHR
The main reason why at all medical facilities need to start using electronic records is to get rid of paperwork. So here are the 7 ‘Whys’ to create EHR software:
- Less routine paperwork. With several clicks, it is possible to find, enter, share, print, and update any data about a patient related to his/her activities.
- Easier management of processes. Online appointments, specialist assignment, data synchronization and transfer, alerts and notifications that can be managed through the system help coordinate and facilitate the workflow.
- All data is stored securely in one place. Paper notes can be easily lost or stolen, while the encrypted data stored and transferred among systems stays safe and is kept away from unauthorized access.
- Enhanced collaboration with colleagues, patients and relatives. Having access to their profiles, patients can quickly get the full information about diagnoses, prescriptions and analyses in digital form remotely and without a necessity to visit a clinic. Good interoperability allows a patient to transfer data seamlessly from one clinic or laboratory to another.
- Less human error. Mistakes cost a lot, and no one is safe from them. It is handy to use an electronic system for filling out prescriptions to reduce the chance of misspelling or having sloppy handwriting errors. As of a study published in PubMed Central, with the introduction of e-prescribing into daily use, error rates decreased from 42% to 7% in one year only!
- Easier communication between patients and medical personnel via secure online chats. Having a chat is a good option for a patient who does not want to wait for an appointment but needs to clarify some quick questions about prescription or diagnosis.
- Easier accounting, reporting and bill sending. Integration with accounting system and insurance companies’ software allows for immediate billing and alerting of patients. This saves your facility a ton of time.
All these advantages have the following positive impact both on your clinic and patients:
- Time and costs reduction due to the automation of numerous tasks and seamless data exchange.
- Quality of medical services improves as data is easily traced and securely stored in one place to be quickly reached and managed remotely.
- Patient satisfaction increases for being able to have their treatment history, lab analyses, prescriptions and payments easily tracked, viewed, sent and printed.
All this sounds just perfect in theory, but what is really going on in practice?
Before we pass to the part on how to create an EMR software or upgrade it up to EHR, let’s consolidate our attention on the challenges that the current users have to deal with for escaping them in future.
What’s Wrong with Your Existing EHR software programs?
90% of physicians use electronic records. Nevertheless, instead of feeling relief from mundane tasks, doctors admit that they are burning out. The struggle with the software made their life more complicated, which resulted in patients being dissatisfied with the service level and multiple doctors making mistakes. Here are the most common issues clinicians indicate when talking about their current EHR software systems:
1. Cumbersome systems prevent staff from effective work
While the main goal of digitizing medical records is to eliminate paperwork, it looks like the documentation burden did not disappear but was just transformed into an electronic version. Moreover, keeping and managing all records in a digital form made the life of physicians even harder than before:
- Unintuitive interfaces lead to physicians burning out, thus increasing the risk of fatal mistakes
First of all, because the systems are too complicated to quickly figure out, it takes even longer to fill all the required fields than just writing some notes by hand (like in the good old days) during the appointment or after work hours. This gives some doctors frustration and stress.
During one 10-hour shift, an ER doctor may do up to 4,000 mouse clicks in EHR, as reported by the American Journal of Emergency Medicine. That’s not very efficient! In research conducted by PlosOne, one of the respondents, a clinician, said:
“It's not really presented in a way that's useful. I always have to click twenty different places to access something. To look at results, I can do it in twenty different ways. Some prefer doing it one way, some prefer doing it another way. That's a little frustrating.”
To top it all off, it was estimated by Annals Family Medicine that doctors spend up to 90 minutes per day after work to make entries into the Electronic Health Record system - cutting into their so-called ‘Pajama Time’. Instead of going home and spending time with family and friends, doctors have to work overtime to complete the records in the EHR.
According to the poll, since the introduction of EHR, a doctor's time on average is dedicated to the following activities:
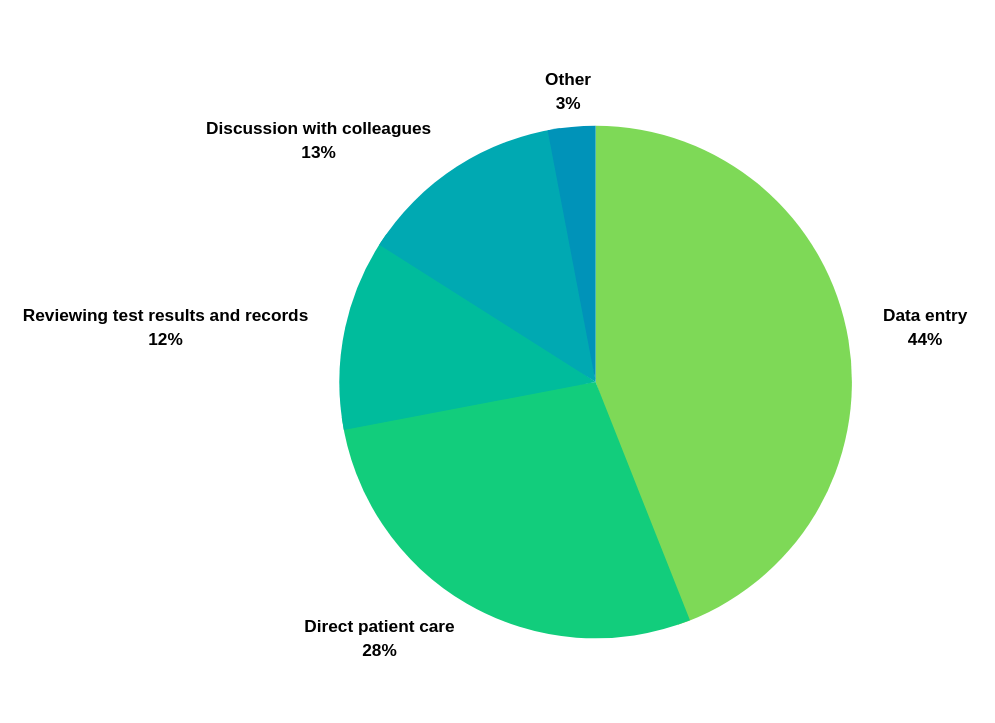
- 44% on data entry,
- 28% in direct patient care,
- 12% reviewing test results and records,
- 13% in discussion with colleagues,
- and 3% in other activities.
Physicians spend more time on records than on the patients who should be their priority. No wonder the patient satisfaction is going down and they are complaining about negligence and inattentive examination during the visits. For that reason only, they may go to a competitor’s clinic where they will have more attention and care.
One of the aims of EHRs is to decrease the number of human errors. However, here we see that the risks are not diminished. On the contrary, the study conducted by MedStar Health’s National Center on Human Factors in Healthcare in three pediatric hospitals resulted in discovering 3,243 mistakes made in prescriptions due to EHR ‘usability issues’. The experiments showed that doctors should be very careful not to make a wrong click. For example, when in the emergency room a doctor orders some medicine and has to select from the drop-down menu with hundreds of options, just one inaccurate action, and selection of the wrong medicine or dosage can cause harm (or even death) to a patient.
Mistakes cost a lot, leading to scandal lawsuits and multimillion fines to clinics.
How do you prevent this? We have some ideas and will share them with you later in this article.
- Workflows and processes are too standardized and inflexible for customization.
Medical institutions are all different and cannot be equalized in processes or in features. That’s why software that doesn't exactly fit the clinic’s working processes may lead to a total mess.
For example, one of the factors that can prevent normal work is excessive alerting. If the personnel receives too many warning signals and notifications on each and every event, they can easily miss a really important message. Between 2014 and 2018, the Joint Commission made an inspection of harmed patients reports to find that 170 incidents (101 of which resulted in patient deaths) happened because of ignorance to alerts because the clinicians had been overloaded with fake and massive alerts!
This is just one of the common issues. Others deal with working processes that do not correspond to the clinic’s routine. Making compromises with software may lead to missing some important steps and result in bad service.
- Poor vendor support and inability to ask for necessary changes in the software.
Though a lot of ready-to-use software can be customized, the logic of some features is still hard-coded and cannot be changed that easily for each individual customer without global changes that affect all other users of the software. That’s why asking your solution vendor for custom rebuilds may be expensive, if possible at all. Also, vendors may change their policies, rebuild their systems or stop supporting some features that are used in your healthcare center. Custom development from scratch gives you full control of your solution and allows 100% flexibility.
2. Insufficient interoperability: data exchange process steals precious minutes that can save lives
- Absence of interoperability with outside organizations because of fierce competition
Another reason why off-the-shelf solutions suck is that they do not provide sufficient interoperability among different clinics’ departments and third-party medical institutions. Hard to believe, but almost 90% of the US EMR providers do not allow for seamless mechanisms of data exchange. That’s either because of competition between software vendors or some technical reasons. If, for example, a patient moves to another city, it may be not easy to seamlessly transfer data from his/her clinics to continue the treatment. This is mostly because clinics do not want to let their patients go to competitors and they try all measures to prevent the ease of data transit.
- Hurdles with data exchange inside organizations
It often happens that one clinic uses several different software that does not share data with each other. This requires additional effort from the personnel to transfer and update information from multiple sources to be on the same page. And sometimes it can even result in a patient’s death. You could hear about the case of Annette Monachelli who died of an aneurysm because the doctor’s order for a head scan had not been transmitted to the lab. This is bad interoperability.
And here is what physicians say about integrations issues they have to struggle with:
“So, in order to get a picture of something, if I need one piece of data that's a lab value and one thing that’s a flow sheet and one thing that’s a radiology thing and one thing that’s an order and one thing that the nurse enters and one thing that the physical therapist enters and one thing that the physician enters, hard. Very very hard, it doesn’t integrate well.”
And sometimes the important data is not on the surface, but hidden in tabs and subtabs, while the system should help the doctor clear the critical and the most up-to-date information from meaningless data.
3. Safety and privacy negligence puts clinics’ reputation at risk and leads to huge fines
According to a JAMIA Open, 1,512 data breaches affecting 154,415,257 patient records were registered from 2013 to 2017 in the United States alone. 128 breaches of those were EMR-related cases and affected 4,867,920 patient records.
Keeping patient data in one place makes things easier, but is at the same time risky. One should make sure that all valuable data is backed up and protected from unauthorized access that could potentially cause harm to patients and the clinic’s reputation.
Of course, it’s not only computers that are to blame when a breach of information happens. The staff themselves put security at risk when they use weak or one-for-all passwords, leave their computer unsupervised and open for visitors' views, do not use antivirus software, leave sticky notes with vulnerable information on the screens of their PCs, etc.
However, the vendor that you work with should also provide all currently existing measures to protect the system and back up the data in case of a system crash.
Need a secure EHR? Let’s discuss your project requirements!
Contact UsHow Can a Custom EHR Solve These Challenges?
The above-listed challenges may seem like enough to detract anyone to create Electronic Healthcare Records software. But the battle is not lost yet. With a complex approach and proper understanding of the aims and challenges, you can obtain a really usable and helpful system that will serve you for many years ahead and save time and money.
Here are 4 areas which a good EHR covers:
1. Creating a well-thought-out, user-friendly UI to reduce doctors’ daily burden
It is important to have an intuitive interface and make automation to mirror your workflow. Doctors should be able to complete their documentation tasks with minimum effort and time wasted. Checklists, handwriting and voice recognition, electronic signature, and some other small but powerful features may significantly increase doctors’ productivity.
Here are some suggestions elaborated by MedStar Health National Center for Human Factors in Healthcare to improve an EHR’s usability and reduce the number of physicians’ mistakes due to ‘usability issues’:
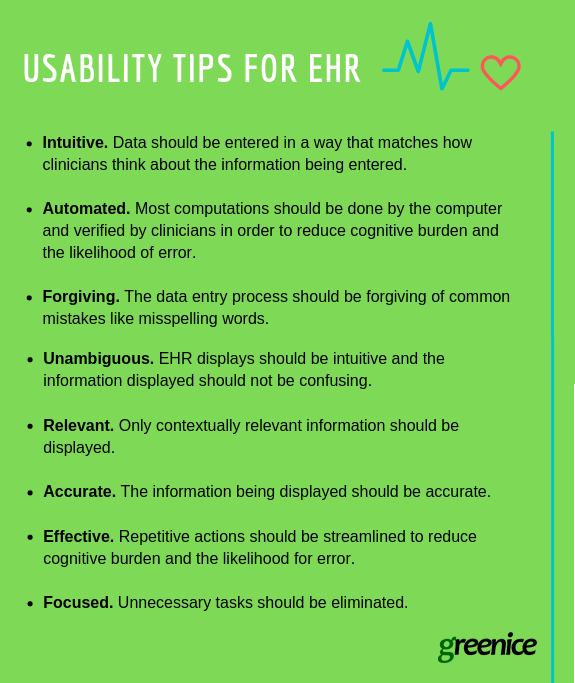
2. Development of unique business logic that responds exactly to your clinic’s workflow necessities
In spite of some similarities, each clinic has its own peculiarities that should be taken into account when creating an EHR.
Custom EHR software development allows you to create a system that does not need to adapt to your workflow; it is already planned from the beginning to function according to the processes that are popular in your medical organization and familiar to your personnel.
Thus, you may include only the features that you need, integrate your software with other systems and decide on any changes during the process.
For example, one of our clients, a mental health counselor agency that provides employee assistance program (EAP) services has absolutely unique workflow.
The agency gives psychological consultations to employees with low efficiency at work (like some physicians that suffer burnout using bad EHRs). To increase efficiency and improve the quality of their services, they needed a system that would consolidate all data and automate routine tasks.
We developed a custom EMR software containing all patients’ data, equipped it with an employer portal to track the therapy results and receive invoices, and an Admin system for in-house and outsourced counselors to assign patients, schedule appointments, and generate reports. This made a perfect combination of several modules with different purposes but tight interoperability.
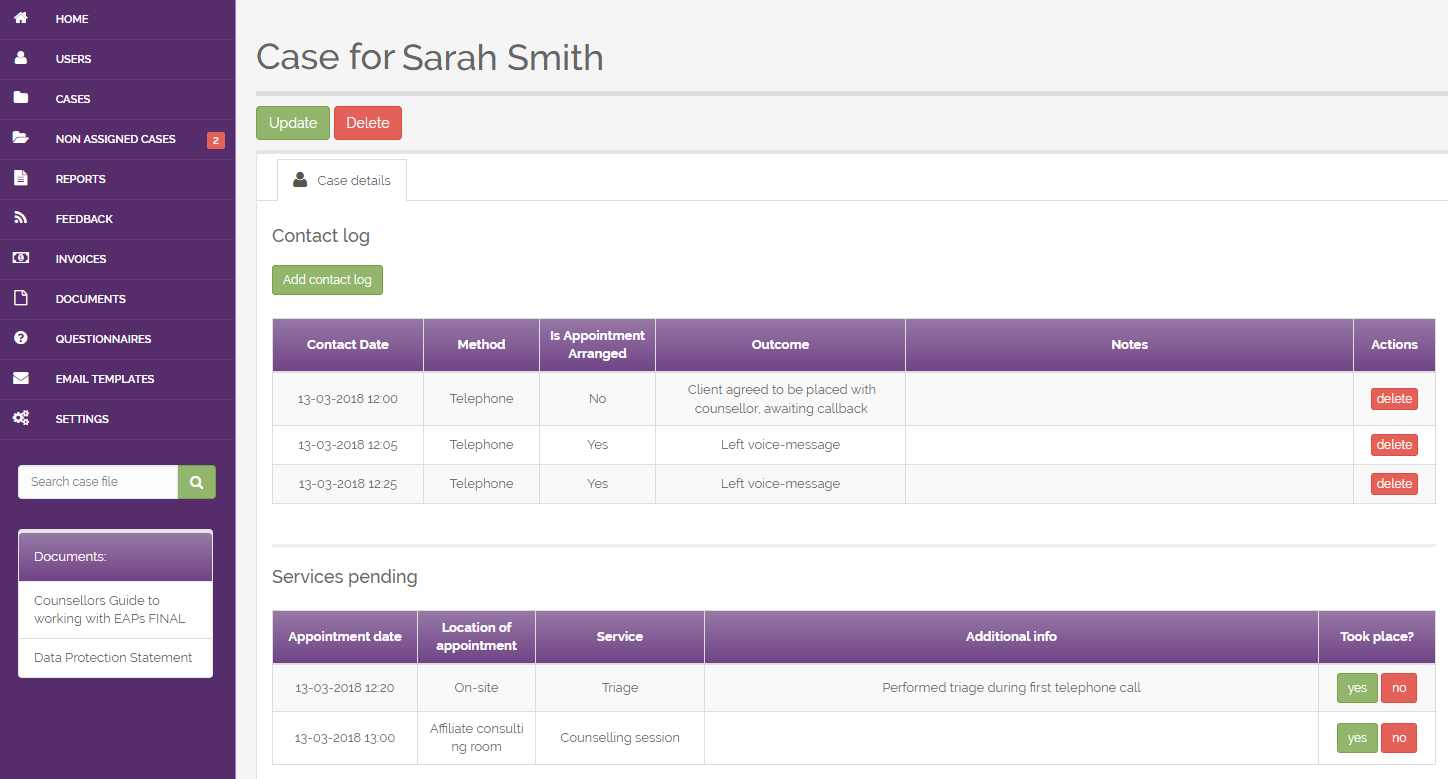
It is definitely hard to find a ready-made solution that is able to fulfill all the specific needs (mental health treatment plan creation, patient state assessment, and reports) and terminology. That’s why a custom approach fully satisfies all the business needs of our customers.
3. Improved exchange between systems to accelerate the data transfer and update
The ability to seamlessly transfer data from one software to another, share data between departments and different medical institutions, give access to patient history and their families can add your practice more points in front of other competitors.
The benefits are:
- Less bureaucracy and time wasted for data transfer
- Less response time due to remote access to data by different departments
- Better diagnostics for the ability to have the full view of the patient’s health
As an example, we will tell you about one of our projects.
One of our clients is a quality home health agency that provides services to people who need assistance and medical care at home. As you can see this is not exactly a medical clinic, so the standard EMR or EHR features and workflows may not fit their needs. They have a portal that combines HRMS, e-Learning, and certification features to facilitate the recruitment and adaptation processes of candidates for caregiving. Providing good interoperability between systems is the key to successful business and customer satisfaction.
4. High level of data security to protect your patients from sensitive data leakage
One of the reasons why it is better to develop custom software rather than use off-the-shelf software is for data security. Big and popular off-the-shelf platforms with many accounts are favorite targets of ‘cybercriminals’ as they can hack a lot of data in bulk with less effort. Of course, attackers try to always be one step ahead of the best protection practices and measures, but compliance with HIPAA regulations, switching on Machine Learning, providing security training for staff, and protecting code with the best-known security measures can prevent breaches.
Here are some of the best practices that should be used for web-based EMR software development, and especially for EHR development:
a) Data storage and backup
Try to use HIPAA compliant data storage for your medical records systems software. We use AWS for HIPAA or TrueVault to guarantee trustworthiness and reliability. Such a system constantly and automatically monitors and updates its security measures and prevents data loss in case of technical issues. As a rule, data is backed up and updated in a separate server to be restored quickly in case of an emergency.
b) User access control
Only authorized and authenticated users should give access to sensitive patient data. User verification by ID, username and password, PIN code, or biometric authentication is a must-have. Also, include automatic logoffs into requirements for your system. In case when a user leaves a workplace without switching off the system, the session will be terminated after a predefined period of time without interaction.
c) Automatic system audit
It is a good practice to log everything that happens in your systems and make automatic reviews of these logs frequently. This helps identify suspicious patterns and risks.
d) Data encryption and authentication
Unfortunately, healthcare systems always remain lucrative targets for hackers that want to either phish out the data to sell it on the black market or to crack the system just for fun.
Encryption is the best way to convert regular data into encoded messages that are impossible to decrypt and read without a key. This is often used for secure data transmission from one source to another (for example, when sending data to a server). There are many techniques of data encryption but both sources (sender and receiver) need to use the same encryption method to work properly. Data sent over a properly authenticated and the secured channel is considered authenticated or verified.
e) Transmission security
You need to protect data that is transmitted from one device or system to another. To do this, use only secure channels for data transmission and encrypt data when possible.
At Greenice, we use modern security practices for data storage, encryption, and anomaly detection and can make your software HIPAA compliant.
How to Make a Custom EMR/EHR That Fits Your Needs
Now that we know the challenges and ways to solve them, let’s put it all together as the steps to follow in both Electronic Healthcare and Electronic Medical Records software development.
Steps for EHR Software Development:
a) Collect the requirements First of all, do not do it on your own. It is a good idea to create a group of people who are going to use the system, as they have a better understanding of what they need and how all the data should work together. This creative group can be further involved in demo sessions and acceptance testing. What you can do is:
- Ask about their current challenges and bottlenecks in their work.
- Try to study their current daily working process.
- Identify the weak areas and find ways of optimizing your existing processes before automating them.
- Do not try to cramp your systems with all of the smallest features possible. Instead, start with the development of high-priority functionalities, test them and then enhance.
It may be difficult for people to find time for the creation of requirements, especially if they need to work. But nevertheless, their participation is necessary.
b) Make a Business Analysis
You can either try to do this by yourself or hire a specialist that will professionally craft a BA for you that will include the challenges and aims of your business, business logic explanation, process optimization, and automation suggestions, wireframes, and features prioritization. Having a Business Analysis allows for quicker and more accurate project estimation. At Greenice, we help you with your Business Analysis.
с) Make a design of your EHR
As bad usability is one of the most critical reasons for physician burnout, it is worth spending time at the very beginning to make clear and logical UI designs. The design should be made before the development will start. Think of mobile and tablet versions. Doctors should be able to make notes and get access to the data on the go. That’s why the interfaces should be easy to use and highly visual. Everything should be on the surface without long paths to get the information.
Many doctors also admit that they would prefer to delegate such tasks as the patient profile creation to the patient’s self-service to save time during the appointment. That’s why having tablet software or remote access is also a good idea.
d) Start development
Each project should have a development plan to follow and timely deliver the product milestones. At each stage of development completion, we organize demo sessions where you and your team can make sure that the project is fulfilled correctly. The features are tested by our QA team and can be delivered to your acceptance testing group for verification.
e) Iterate It is always better to deliver the first version quicker to have a chance to test it and find ways to improve. That is why the prioritization of features is so important. After a project launch, we can continue maintenance and work on improvements.
Do you need help with Business Analysis?
Contact Us Now!How to Apply This to Your Business
The aim of our article was to demonstrate that you are not alone in your struggle with off-the-shelf EHR issues. There are many companies that are similarly not satisfied or even became the victims of inefficient work of their system.
We also wanted to show you that we differentiate medical organizations by their types and treat each business individually with your needs in mind to propose the best solution. Whether you are a hospital, private practice, caregiving agency, assisted living facility, nursing home, mental health counseling center or other kinds of medical service, we can find the right solution for you.
Here is a shortlist of what you can already do now:
- Ask your personnel about the hurdles in their work with existing software
- Go through the current workflow of different employees and optimize the business processes
- Brainstorm with colleagues on what should be automated or changed in the existing solution, or if you do not use EHR yet, what features you would like to have
- Make or order Business Analysis from the specialists. At Greenice, we can help you with the Business Analysis.
- Find a designer with good command in medical systems usability
- Send requirements and designs to us for estimation
- Start development and gradually enhance features
Do you want to send us your requirements and get a free quote?
Contact Us Now!Rate this article!
Not rated












 Sign in with Google
Sign in with Google
Comments (0)